Madhumathi Subramanian, BS Opt, FCL, FIACLE, FSLS, FBCLA
Deputy Manager – Department of Contact Lens, Sankara Nethralaya, Chennai, India
Assistant Professor, Elite School of Optometry and The Sankara Nethralaya Academy, Chennai, India
Abstract
Scleral contact lenses provide exceptional visual rehabilitation and ocular surface protection, particularly in patients with irregular corneas and ocular surface disorders. Despite their effectiveness, many practitioners perceive scleral lens fitting as complex and dependent on advanced instrumentation such as corneoscleral profilometers or Anterior Segment Optical Coherence Tomography (AS-OCT). Evidence indicates that accurate fitting outcomes can be achieved using structured diagnostic fitting approaches, slit-lamp evaluation, and careful clinical observation, making scleral lens practice highly user-friendly.
This review summarises practical strategies for estimating central vault, limbal clearance, and scleral alignment, decision-making for haptic modifications, initial sagittal height and lens diameter selection, front surface eccentricity, optic zone considerations, and lens centration. By emphasising clinical judgment over instrumentation, practitioners can achieve safe and effective scleral lens wear while enhancing visual quality and patient satisfaction.
Keywords: scleral lens fitting, clinical observation, vault assessment, limbal clearance, haptic modification, lens centration, front surface eccentricity
Introduction
Scleral lenses have become a mainstay in managing irregular corneas and ocular surface disorders due to their ability to provide stable optics, comfort, and ocular surface protection. Although technological advancements such as AS-OCT and profilometers can quantify vault and alignment, most successful fits are achieved through careful clinical evaluation. A structured, observation-based technique combined with diagnostic lens sets enables practitioners to rely on slit-lamp assessment, fluorescein evaluation, and patient feedback.

Figure 1: Scleral Lens
Clinical Estimation of Vault and Limbal Clearance
Central vault is critical for avoiding corneal touch and maintaining a healthy post-lens tear film. The initial sagittal height can be selected based on the corneal contour: ectatic corneas require higher sagittal heights, whereas normal corneas may be fitted with lower values. Lens diameter is guided by the Horizontal Visible Iris Diameter (HVID), ocular surface anatomy, and severity of ectasia.
Using a slit-lamp, practitioners estimate vault by observing the fluorescein-stained post-lens tear reservoir. Since lenses settle by approximately 80–150 µm during the first few hours, an initial vault of 300–400 µm typically ensures a safe settled vault of 150–250 µm (Figure 2A & 2B). Limbal clearance must be confirmed to protect the palisades of Vogt, as limbal touch may compromise stem cell function. (1,2)

Figure 2: A. Central Vault, B. Limbal Vault
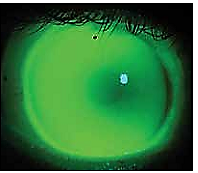
Figure 3: Limbal Touch
Haptic Adjustments and Decision-Making
Edge alignment is assessed by observing conjunctival blanching, indentation, or vessel impingement. Mild haptic misalignment may normalise after settling, but immediate vessel impingement (Figure 4) requires prompt modification such as flattening or using toric haptics. Studies confirm that clinical decisions made through slit-lamp evaluation yield reliable outcomes, even without advanced imaging. (3)
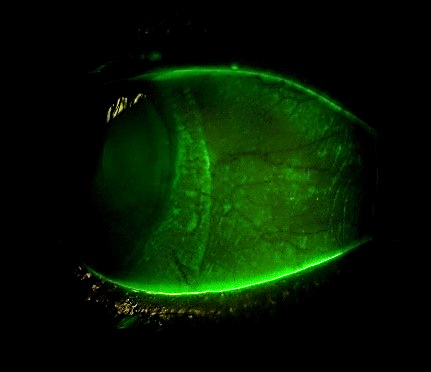
Figure 4: Conjunctival Impingement
Lens Centration, Front Surface Eccentricity and Optic Zone Selection
Scleral lenses often decentre temporally due to scleral asymmetry and extraocular muscle influence. Proper diameter, landing zone width, and haptic geometry help minimise decentration. (4) Front surface eccentricity adjustments may improve clarity in patients with irregular corneas by reducing ghosting. For decentred lenses, selecting larger optic zones ensures the visual axis remains covered.
In patients with ocular surface disease and relatively preserved acuity, front surface eccentricity and optic zone customisation significantly improve visual satisfaction.
Diagnostic Lens Sets and Practical Strategies
Diagnostic trial lens sets remain the gold standard for evaluating vault, haptic alignment, limbal clearance, and visual performance. Empirical calculators and manufacturer consultation further support clinical decision-making. (5) Patient feedback continues to be vital, particularly when assessing comfort and visual sharpness.
Conclusion
Scleral lens fitting can be simplified by combining structured diagnostic lens evaluation, slit-lamp observation, and practical clinical judgment. Accurate fitting and optimal visual outcomes are achievable without advanced imaging tools, provided practitioners systematically assess vault, limbal clearance, haptic alignment, sagittal height, diameter, centration, eccentricity, and optic zone size. This approach ensures safe, comfortable, and effective scleral lens wear, making specialty contact lens practice accessible to a wide range of clinicians.
Declaration of Interest: This blog is written solely for academic and educational purposes. There is no financial support or conflict of interest.
References
- Michaud L, Lipson M, Kramer E, et al. The official guide to scleral lens terminology. Cont Lens Anterior Eye. 2020;43(4):529–534.
- Vincent SJ, Collins MJ, Alonso-Caneiro D. The rigid lens renaissance: a surge in sclerals. Cont Lens Anterior Eye. 2018;41(2):139–143.
- Schornack MM. Scleral lenses: a literature review. Eye & Contact Lens. 2015;41(3):3–11.
- Walker MK, Bergmanson JP, Miller WL, Marsack JD, Johnson LA. Complications and fitting challenges associated with scleral contact lenses. Cont Lens Anterior Eye. 2016;39(2):88–96.
- Shorter E, Harthan J, Nau CB, et al. Scleral lenses in the management of ocular surface disease. Eye & Contact Lens. 2018;44(4):372–378.
About the Author

With over 19 years of experience, Ms. Madhumathi specialises in clinical refraction, specialty contact lens fitting, and optometric education. She serves as a senior contact lens practitioner at Sankara Nethralaya, India’s No. 1 eye hospital, where they manage more than 6,000 regular cornea and 4,000 irregular cornea cases annually. Her expertise spans the full spectrum of speciality contact lenses, including scleral, hybrid, orthokeratology, and prosthetic lenses.
She holds a Bachelor of Science in Optometry from the Elite School of Optometry (affiliated with BITS Pilani, 2004) and a Fellowship in Contact Lenses from The Sankara Nethralaya Academy (2011). She is a Fellow of the International Association of Contact Lens Educators (FIACLE, 2024), the Scleral Lens Education Society (FSLS, 2024), and the British Contact Lens Association (FBCLA). Her experience also includes FDA-approved clinical trials, with a strong focus on orthokeratology and scleral lenses.
As an Associate Professor, she mentors undergraduate and postgraduate optometry students in contact lens and low vision research projects. Her research interests centre around speciality lens fitting for irregular corneas, and she has served as a co-investigator in three FDA clinical trials.
Ms. Madhumathi is a frequent speaker at international conferences, including IACLE, ICLEP, and BCLA, and has led numerous speciality contact lens workshops. She was honoured as the IACLE Contact Lens Educator of the Year 2024 (Asia Pacific) and received the Hospital Optometry Practitioner of the Year Award at BCLA 2025, where she was also invited as a guest speaker to present her research.
Selected Publications:
- PROSE for Irregular Corneas – Eye & Contact Lens (2014)
- Custom Soft Toric Lenses – Contact Lens Spectrum (May 2014)
- Tear Ascorbic Acid & Antioxidant Status in CL Wearers – Indian Journal of Ophthalmology (2009)
- Bilateral Keratoconus with Granular Dystrophy: A Case Report – Indian Journal of Ophthalmology (2024)
- Scleral Lenses in Limbal Stem Cell Deficiency – Indian Journal of Ophthalmology (2024)
- Piggyback Scleral Lenses in Stevens-Johnson Syndrome – Eye & Contact Lens (2025)
- Cost and Benefits of Specialty Contact Lenses – Contact Lens & Anterior Eye (2025)


Recent Comments