Rupali, D. Optom, B. Optom, F. Optom, M. Optom, FDP USA
Consultant Paediatric Optometrist – Cerebral Visual Impairment and Binocular Vision, Save Sight Centre, Delhi, India
Abstract
Cerebral Visual Impairment (CVI) is the most common cause of paediatric visual impairment in both developed and developing countries. With the advent of improved neonatal care, the survival rate of preterm and neurologically compromised infants has increased, which in turn has led to a higher incidence of CVI. This article discusses the clinical presentation, aetiologies, comorbidities, diagnostic challenges, and the importance of a multidisciplinary, optometry-led approach for early detection and intervention. Based on current evidence and aligned with findings from the Indian Journal of Ophthalmology’s multicentric study (Mohapatra et al., 2022), this article emphasises the need for increased awareness, timely referrals, and structured rehabilitation protocols. (1)
Introduction
Cerebral Visual Impairment (CVI), also known as Cortical Visual Impairment, is a neuro-ophthalmic disorder characterised by impaired visual function due to damage in the post-geniculate visual pathways of the brain. Unlike ocular blindness, CVI presents with structurally normal eyes but abnormal visual behavior and perception. As highlighted by Mohapatra et al. (2022), the prevalence of CVI is on the rise, particularly due to improved survival of neonates with hypoxic-ischemic encephalopathy (HIE), neonatal seizures, and other neurological insults. (1)
Clinical Presentation and Functional Impact
Children with CVI often present with diverse symptoms such as:
- Inconsistent visual responses
- Difficulty recognising faces, objects, or navigating through cluttered spaces
- Preference for peripheral vision
- Gazing
- Simultagnosia
- Attraction to moving or high-contrast stimuli (especially red)
- Sensitivity or fascination with light sources
These behaviors are frequently misunderstood, leading to delayed diagnosis or mis-labeling as developmental delay or autism. (2) The Indian multicentric study by Mohapatra et al. reported significant ocular comorbidities, including refractive errors (63.2%), strabismus (60.2%), and optic atrophy (25.9%), all contributing to variable visual outcomes. (1)
Associated Comorbidities
CVI is commonly associated with:
- Seizure disorders (50.4%)
- Cerebral palsy (13.6%)
- Developmental delay (80.5%)
- Hearing loss, microcephaly, and autism spectrum disorders
The study emphasised that optic atrophy and seizure disorders are strong predictors of severe visual impairment (<20/200), with odds ratios of 2.6 and 2.1 respectively (p < 0.05).
Etiological Factors
The leading causes identified include:
- Hypoxic-ischemic encephalopathy (35.1%)
- Seizure-associated brain injury (31.3%)
- Neonatal hypoglycemia (10.9%)
- Structural brain anomalies (9.6%)
- Hypocalcemia
These findings align with global literature but also underscore the need for early neurological screening in neonates at risk(3).
Diagnostic Approach
Optometrists, ophthalmologists, and paediatric neurologists must collaborate for timely CVI diagnosis. Key steps include:
- Comprehensive paediatric ocular examination, including detailed birth history in all paediatric groups
- Functional vision testing and observation of visual behavior including contrast, visual field and cognitive skills
- Right choice of cycloplegic refraction to detect uncorrected refractive errors and anterior posterior eye examination
- Use of tools such as the CVI Range or CVI-specific behavioral check-lists with typical sign and symptoms
- Neuro-imaging (e.g., MRI) to assess structural anomalies and part of brain involvement
- Electroencephalogram (EEG) also help to detect lobe involvement and damage
Children with disproportionate visual deficits relative to ocular findings should be evaluated for CVI.
Management Strategies
Management should be tailored to the child’s visual profile and include:
- Correcting refractive errors
- Prescribe right choice of glasses as few of them also have sensory issues
- Structured vision therapy, visual stimulation activities and vision rehabilitation
- Environmental adaptations (decluttering, colour contrast enhancement)
- Sometimes, they may need low vision devices as well
- Parent training to reinforce visual engagement therapy and environmental modification
- Multi-sensory integration therapy
- They may need Occupational Therapy and Physiotherapy
Evidence from the Indian multicentric study supports the utility of individualised rehabilitation in improving functional vision outcomes. (4)
Interdisciplinary Model for CVI Assessment
- Early risk-based screening
- Functional and behavioral vision assessments
- Visual habilitation plans across CVI levels
- Family and educator collaboration
- Regular follow-up and neuro-ophthalmic liaison
We advocate a proactive approach, aligning with Mohapatra et al.’s recommendation for early diagnosis to prevent amblyopia and support developmental milestones. (1)
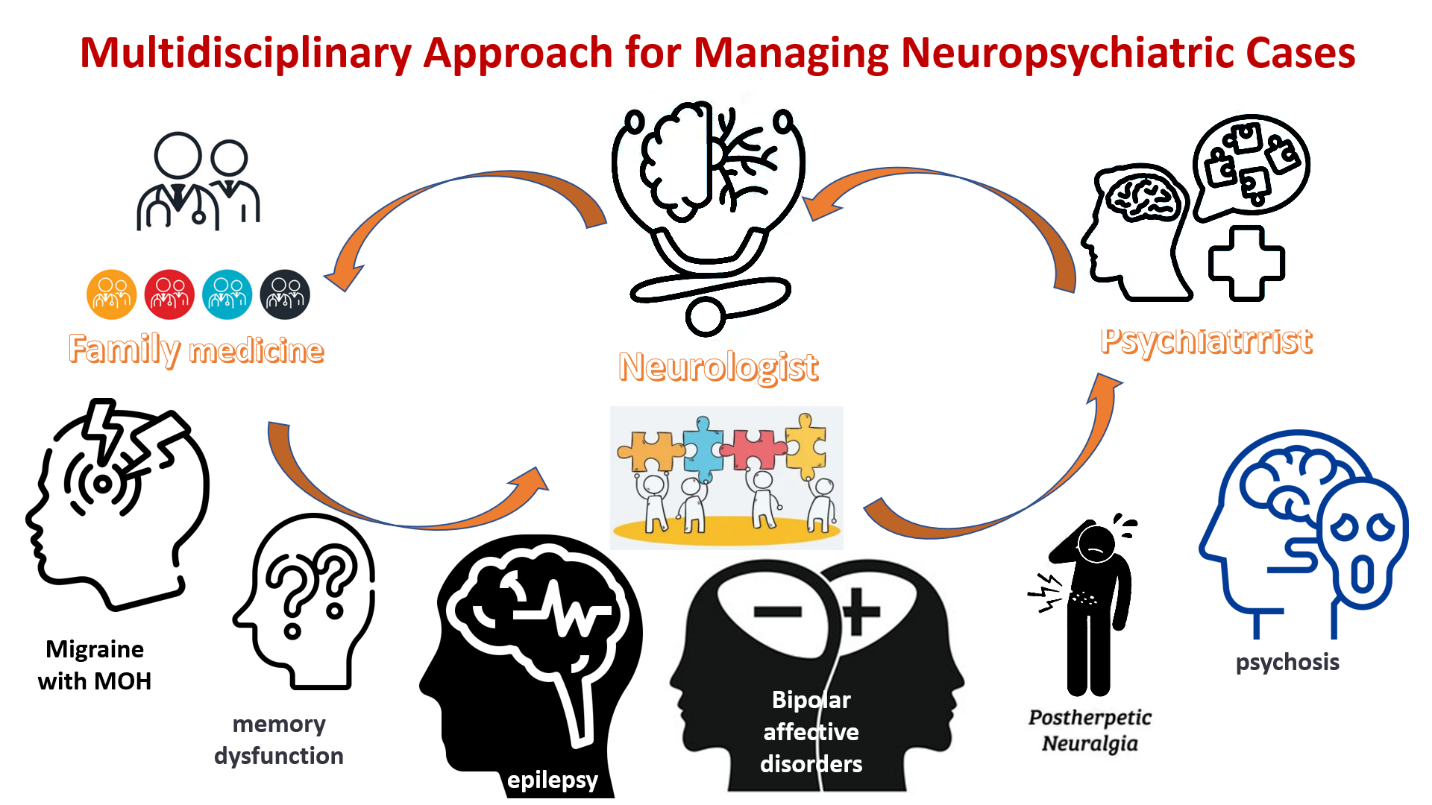
Figure 1: Managing CVI patient
Conclusion
CVI poses a significant challenge in paediatric visual health. The burden is under-estimated due to diagnostic complexities and low awareness among front-line clinicians. With data from large-scale studies like Mohapatra et al. (2022), it is evident that early detection, multidisciplinary collaboration, and functional rehabilitation can improve visual outcomes. Paediatric optometrists play a pivotal role in screening, diagnosis, and long-term management. Future directions should focus on standardised screening protocols, clinician training, and care-giver education to mitigate the long-term impact of CVI. (1)
References
- Mohapatra M, Rath S, Agarwal P, et al. Cerebral visual impairment in children: Multicentric study determining the causes, associated neurological and ocular findings, and risk factors for severe vision impairment. Indian J Ophthalmol. 2022;70(12):4410-4415.
- Huo R, Burden S, Hoyt CS, Good WV. Chronic cortical visual impairment in children: Etiology, prognosis, and associated neurological deficits. Br J Ophthalmol. 1999;83:670-675.
- Pehere N, Chougule P, Dutton GN. Cerebral visual impairment in children: Causes and associated ophthalmological problems. Indian J Ophthalmol. 2018;66:812-815.
- Roman-Lantzy C. Cortical Visual Impairment: An Approach to Assessment and Intervention. AFB Press.
- Ganesh S, Khurana R, Sharma S, Rath S. Predisposing factors, ophthalmic manifestations, and radiological findings in children with cerebral visual impairment. J Pediatr Ophthalmol Strabismus. 2019;56:313-318.
Author:-

Ms Rupali is a Consultant Optometrist specialising in Paediatric CVI, Binocular Vision & Neuro-Rehabilitation. She was awarded Best Optometrist for clinical and academic excellence and received Best Student Award and Topper Merit Certificate from St. Stephen’s and Sharda University in 2017. In 2019 she completed a Fellowship in Paediatric Orthoptic Binocular Vision & Vision Therapy at Dr. Shroff Charity Eye Hospital. From 2019–2024 she served as Senior Paediatric & CVI Optometrist and myopia expert at Dr. Shroff’s Charity Eye Hospital, Daryaganj. In 2021 she got certified in CVI and Vision Therapy from Narayana Nethralaya and completed FDP in CVI and Seizure Safety Care (USA) in 2024. Currently, she serves as a Consultant Optometrist at Save Sight, leading the Paediatric CVI & Binocular Vision Department and Vision Therapy
In 2023, she was appointed as the Central Representative President and Education Committee Member of the Delhi Optometry Association (DOA).
She has published extensively in national and international journals and contributed as a speaker at major conferences across India and abroad. She has also trained numerous optometry fellows and junior ophthalmologists. Rupali conducts webinars and online training programs and is known for her empathetic patient care and evidence-based therapy. She is highly praised by patients and peers for her clinical excellence.

Recent Comments