Yukti D. Pandya, M. Optom
Optometry Faculty, SNDT Women’s University, Mumbai, India
Visual Snow Syndrome (VSS), identified in 1995, is characterised by persistent flickering or pixelation across the visual field, significantly impacting daily activities. It commonly begins in young adulthood but may occur at any age. VSS is defined by continuous “visual snow” along with at least two additional visual symptoms. Although typically benign and non-progressive, it may be associated with ocular or neurological disorders. (1)
Clinical Features
Vision plays a central role in VSS. Patients experience constant grainy noise throughout their visual field, even in complete darkness. Common visual symptoms include:
- Palinopsia: Afterimages and trailing of moving objects.
- Enhanced entoptic phenomena: Increased awareness of natural visual effects.
- Blue field entoptic phenomena: Bright moving white dots seen against blue sky.
- Spontaneous photopsia: Sudden flashes of light.
- Nyctalopia: Difficulty seeing in dim light.
- Photophobia: Sensitivity to light.
- Visual distortions: Halos, metamorphopsia, moving lines, coloured clouds, even with eyes closed.
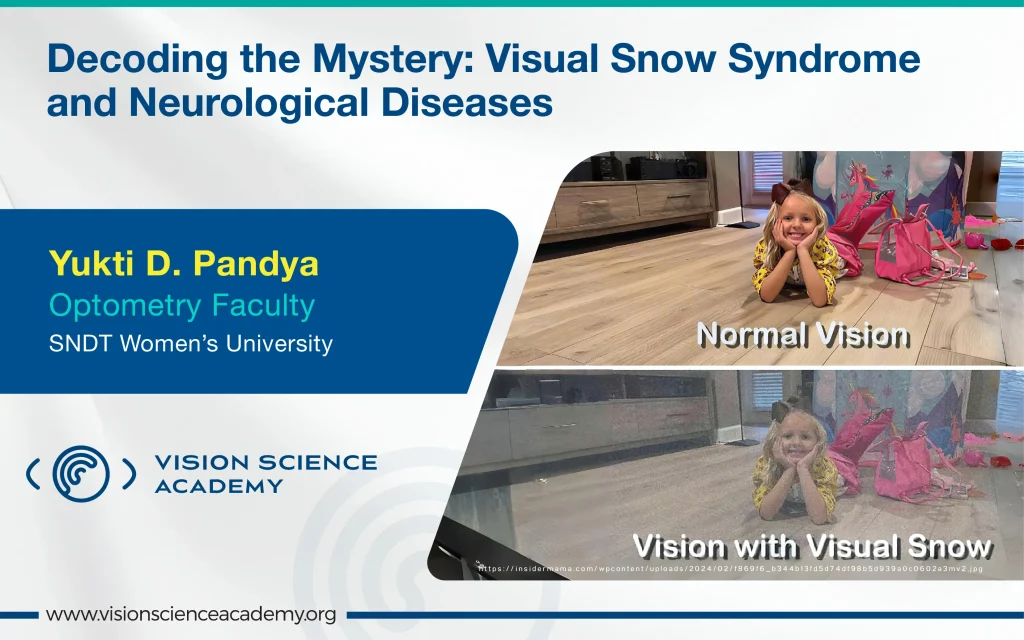
Figure 1: Visual Snow Syndrome
The biological mechanisms of VSS are not fully understood. Much of the available information comes from case reports and small study samples. (2)
Pathophysiology
The pathophysiology of VSS is not fully understood but involves abnormalities in the V1 and V2 areas of the occipital cortex, leading to hallucinations and increased grey matter in visual regions. There are alterations in connectivity within visual and attention pathways and changes in visual evoked potentials.
Impaired thalamocortical dysrhythmia may play a role in VSS due to heightened activity in the Lateral Geniculate Nucleus (LGN) or pulvinar. The connection between the pulvinar and lingual gyrus is associated with photophobia and visual filtering difficulties, with some patients benefitting from coloured filters that block blue wavelengths. (3)
VSS Correlation with Neurological Disease
Charles Bonnet Syndrome (CBS) involves visual hallucinations in individuals with severe vision loss, affecting 40–60% of those with conditions like glaucoma or age-related macular degeneration. Hallucinations vary based on visual processing pathways. (4)
Migraine patients often experience VSS, with up to 80% sharing symptoms. fMRI studies show altered Blood Oxygen Level Dependent (BOLD) activity related to visual disturbances. VSS patients have reduced BOLD responses, and photophobia is linked to specific brain areas. Additionally, patients with retinitis pigmentosa show increased awareness of photopsia. (4,6)
Neurological issues like stroke, epilepsy, multiple sclerosis, tumours, and degenerative disorders can cause visual snow, typically noted in the medical history of the patients. While episodic visual snow can occur in migraine and occipital lobe epilepsy, it does not meet the criteria for VSS. VSS, common in concussions or brain injuries, is characterised by persistent pixelated “visual snow” in the visual field, either in grayscale or colour. (4,5)
Treatment
Many patients declined treatment and medication due to manageable symptoms or fear of side effects. Tinted lens assessments show that VSS patients often benefit from blue-yellow filters. Some studies suggest partial relief with medications like lamotrigine, topiramate, benzodiazepines, and acetazolamide. (6)
Conclusion
Visual Snow Syndrome is a neurological condition characterised by continuous visual static and associated disturbances such as palinopsia and photophobia. Although the exact cause remains unclear, current evidence indicates abnormal brain activity within key visual processing regions. While no definitive cure exists, patients may find relief using tinted lenses or specific medications. Continued research is essential to understand VSS better and develop effective treatments.
References
- Traber, G. L., Piccirelli, M., & Michels, L. (2020). Visual snow syndrome: a review on diagnosis, pathophysiology, and treatment. Current Opinion in Neurology, 33(1), 74–78.
- Kondziella, D. (2022). Visual snow syndrome and the emperor’s new clothes. Brain Communications, 4(4), fcac178.
- Fraser, C. L. (2022). Visual snow: updates on pathology. Current Neurology and Neuroscience Reports, 22(3), 209–217.
- Fraser, C. L. (2024). How do I recognise and manage visual snow syndrome? Eye, 38(12), 2253–2256.
- Ciuffreda, K. J., Han, M. E., Tannen, B., & Rutner, D. (2021). Visual snow syndrome: evolving neuro-optometric considerations in concussion. Concussion, 6(2), CNC89.
- Yoo, Y. J., Yang, H. K., Choi, J. Y., Kim, J. S., & Hwang, J. M. (2020). Neuro-ophthalmologic findings in visual snow syndrome. Journal of Clinical Neurology, 16(4), 646.