Raghul Gurunathan, B. Optom., FBV and VT
Optometrist and Vision Therapist, Divine Myndz Vision Care and Therapy Centre, Chennai, India
The Hemifield slide phenomenon is a non-paretic diplopia caused by disrupted fusion between visual hemifields in heteronymous field loss. It results from the loss of corresponding retinal points, allowing a latent phoria to manifest as misalignment. Most often linked to bitemporal hemianopia from optic chiasm lesions (e.g., pituitary adenoma, suprasellar mass), it can also occur with heteronymous altitudinal defects or binasal hemianopia. (1)
Mechanism
- Normal binocular vision relies on nasal-temporal field overlap, forming corresponding retinal points for fusion and single vision. (1,2)
- In heteronymous hemianopia, overlap is lost, disrupting correspondence, making latent phoria manifest as tropia. (1,2)
- This causes hemifields to “slide” horizontally or vertically, producing binocular diplopia. (1,2)
Causes
| Visual Field Defect | Mechanism | Common Causes |
|---|---|---|
| Bitemporal Hemianopia | Lesion at optic chiasm disrupts nasal retinal fibers → temporal field loss → loss of fusion. |
|
| Heteronymous Altitudinal defect | Horizontal meridian defect → vertical fusion disruption. |
|
| Binasal Hemianopia | Bilateral nasal field loss (temporal retina) → central overlap lost → fusion failure. |
|
Table 1: Visual Field Defects related to Hemifield Slide – Mechanisms and Common Causes
Ocular Manifestations
Depending on the type of underlying phoria, the visual symptoms may vary:
- Exodeviation: Perception of a doubled or overlapping central strip of vision, due to outward divergence and relative outward displacement of the visual fields. (8) (Eg: Fig 1. B)
- Esodeviation: Appearance of a central gap, blank area, or missing portion, caused by inward turning of the eyes with overlapping suppression zones and loss of central fusion. (8) (Eg: Fig 1. C)
- Vertical deviation: Vertical misalignment of the hemifields, where one image is perceived above the other, producing a “split” effect. (8) (Eg: Fig 1. D)
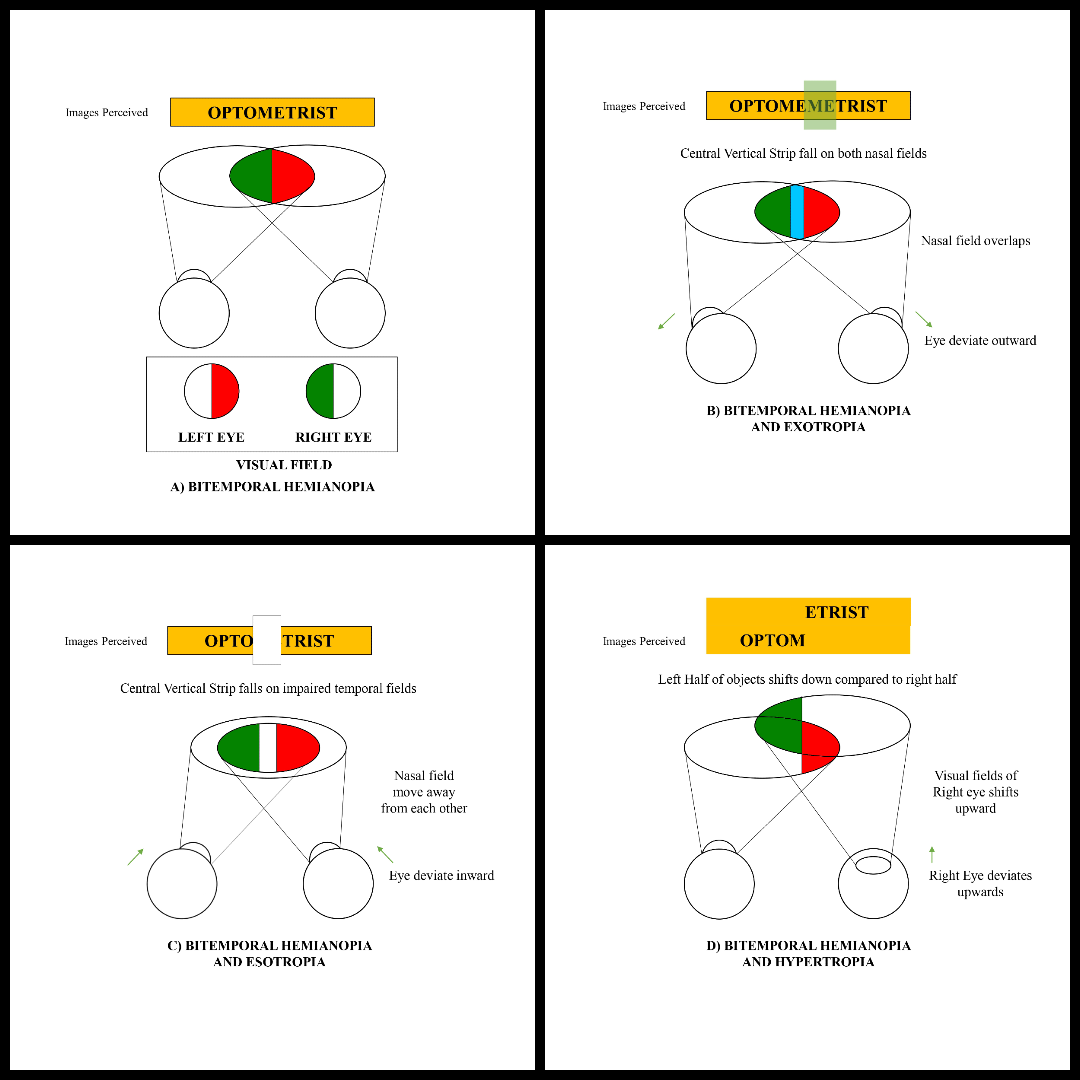
Figure 1: Schematic of Hemifield Slide
Diagnostic Approach
Visual field testing (Humphrey/Goldmann) detects heteronymous defects, cover tests reveal tropia/phoria, Magnetic Resonance Imaging (MRI) identifies chiasmal lesions, and fundus imaging/Optical Coherence Tomography (OCT) shows optic nerve changes with Retinal Nerve Fiber Layer (RNFL)/Ganglion Cell Layer (GCL) loss. (2,9)
Management
-
Treat Underlying Cause
- Resectable brain lesions (e.g., pituitary macroadenoma) are best managed by surgical removal. (6)
- Visual field defects and diplopia may resolve post-surgery. (6)
- If surgery is not feasible or symptoms persist, visual rehabilitation is advised. (6)
-
Orthoptic Therapy
- Fusional convergence exercises help control ocular deviation. (3)
- Sectoral prism glasses may be prescribed to maintain binocular vision. (3)
-
Surgical or Medical Intervention
- Botulinum toxin injections into extraocular muscles have been attempted, with inconsistent results. (3)
- Strabismus surgery may be considered in select cases, though outcomes vary. (3)
Conclusion
Hemifield slide phenomenon is a rare binocular vision disturbance, most often seen in bitemporal hemianopia with ocular deviation. It results from misalignment of the two hemifields, leading to a shift or duplication of the visual field. Since the condition disrupts binocular fusion, accurate diagnosis is crucial for effective management.
References
- Peragallo, J. H., Bialer, O. Y., Pineles, S. L., & Newman, N. J. (2014). Hemifield Slide Phenomenon as a Result of Heteronymous Hemianopia. Neuro-Ophthalmology, 38(2), 82–87.
- van Waveren, M., Jägle, H., & Besch, D. (2013). Management of strabismus with hemianopic visual field defects. Graefe’s archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie, 251(2), 575–584.
- Peli, E., & Satgunam, P. (2014). Bitemporal hemianopia; its unique binocular complexities and a novel remedy. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists), 34(2), 233–242.
- Foroozan R. (2016). Visual Findings in Chiasmal Syndromes. International ophthalmology clinics, 56(1), 1–27.
- Maniec, K., & Watson, J. C. (2011). Spontaneous Rupture, Disappearance, and Reaccumulation of a Rathke’s Cleft Cyst. Case reports in endocrinology, 2011, 549262.
- Pula, J. H., & Yuen, C. A. (2017). Eyes and stroke: the visual aspects of cerebrovascular disease. Stroke and vascular neurology, 2(4), 210–220.
- Borchert, M. S., Lessell, S., & Hoyt, W. F. (1996). Hemifield slide diplopia from altitudinal visual field defects. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society, 16(2), 107–109.
- Shainberg, M. J., Roper-Hall, G., & Chung, S. M. (1995). Binocular problems in bitemporal hemianopsia. American Orthoptic Journal, 45(1), 132–140.
- Foroozan R. (2016). Visual Findings in Chiasmal Syndromes. International ophthalmology clinics, 56(1), 1–27.

Recent Comments