Prattoy Bej, F. Optom
Clinical Optometrist, Dr. Shroff’s Charity Eye Hospital, New Delhi, India
Fundus examination inspection of the back of the eye (the fundus) offers clinicians a unique, non-invasive window into the body’s vascular and neurological health. Its value extends well beyond ophthalmology, supporting early detection and monitoring of systemic disease. (1)
Importance of Fundus Examination
Direct Visual Access to Blood Vessels: The fundus is one of the only locations in the human body where blood vessels and neural tissue can be directly observed without invasive procedures. (1)
Early Detection of Systemic Disease: Retinal vascular or optic nerve changes can signal systemic disease—sometimes before symptoms appear elsewhere. (2,3)
Monitoring Disease Activity: In chronic conditions such as hypertension, diabetes, or autoimmune disorders, fundus findings may reflect severity and progression and can help assess treatment response. (3)
Infectious Diseases
Systemic infections including septicaemia, endocarditis, Human Immunodeficiency Virus (HIV), tuberculosis, syphilis, and candidemia can produce characteristic fundus findings. These may include retinal haemorrhages, vasculitis, and distinctive lesions. Importantly, fundus abnormalities can appear before overt systemic symptoms in some patients, making fundus examination a potentially life-saving tool in at-risk individuals. (2)
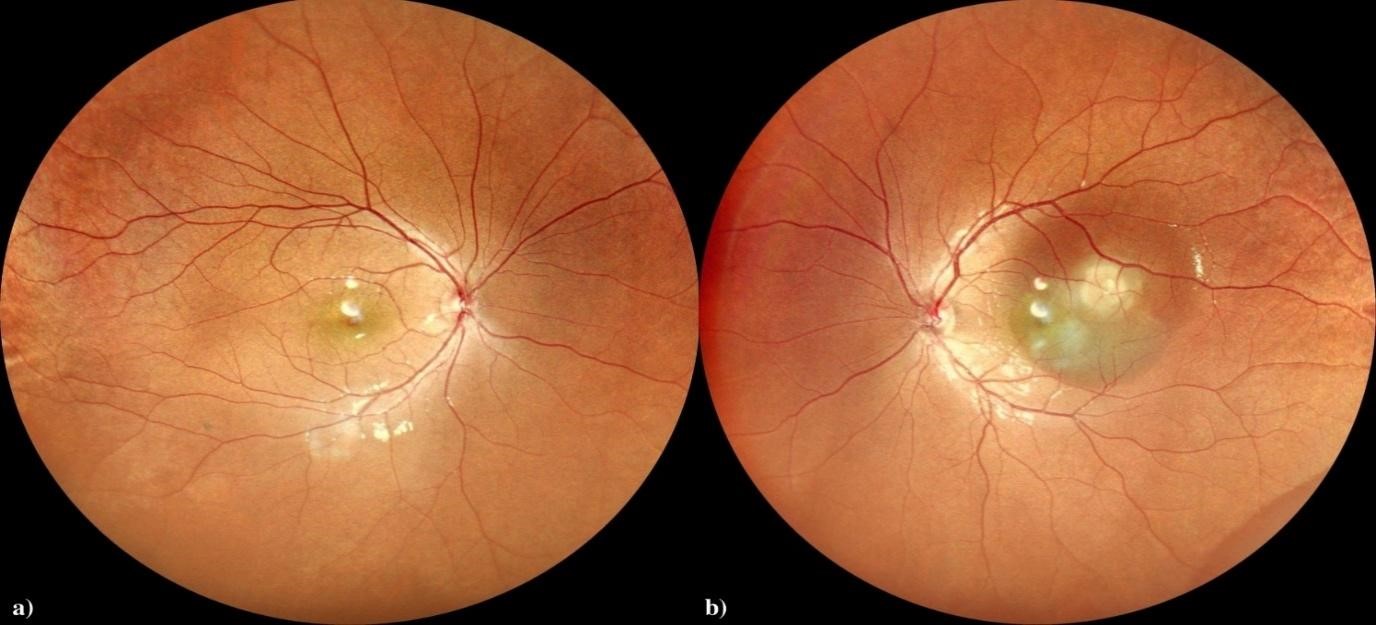
Figure 1: Fundus Image of a Tuberculosis Granuloma Patient
Autoimmune Diseases
In Systemic Lupus Erythematosus (SLE), ocular involvement is common. Fundus changes such as retinopathy and choroidopathy suggest microvascular and structural damage to the retina and choroid. These findings can correlate with systemic disease activity particularly involvement of organs such as the kidneys and brain—and may occasionally be the earliest manifestation of SLE, occurring before other systemic symptoms. (3)

Figure 2: Slit Lamp Photograph Demonstrating Diffuse Anterior Scleritis in a Patient with SLE
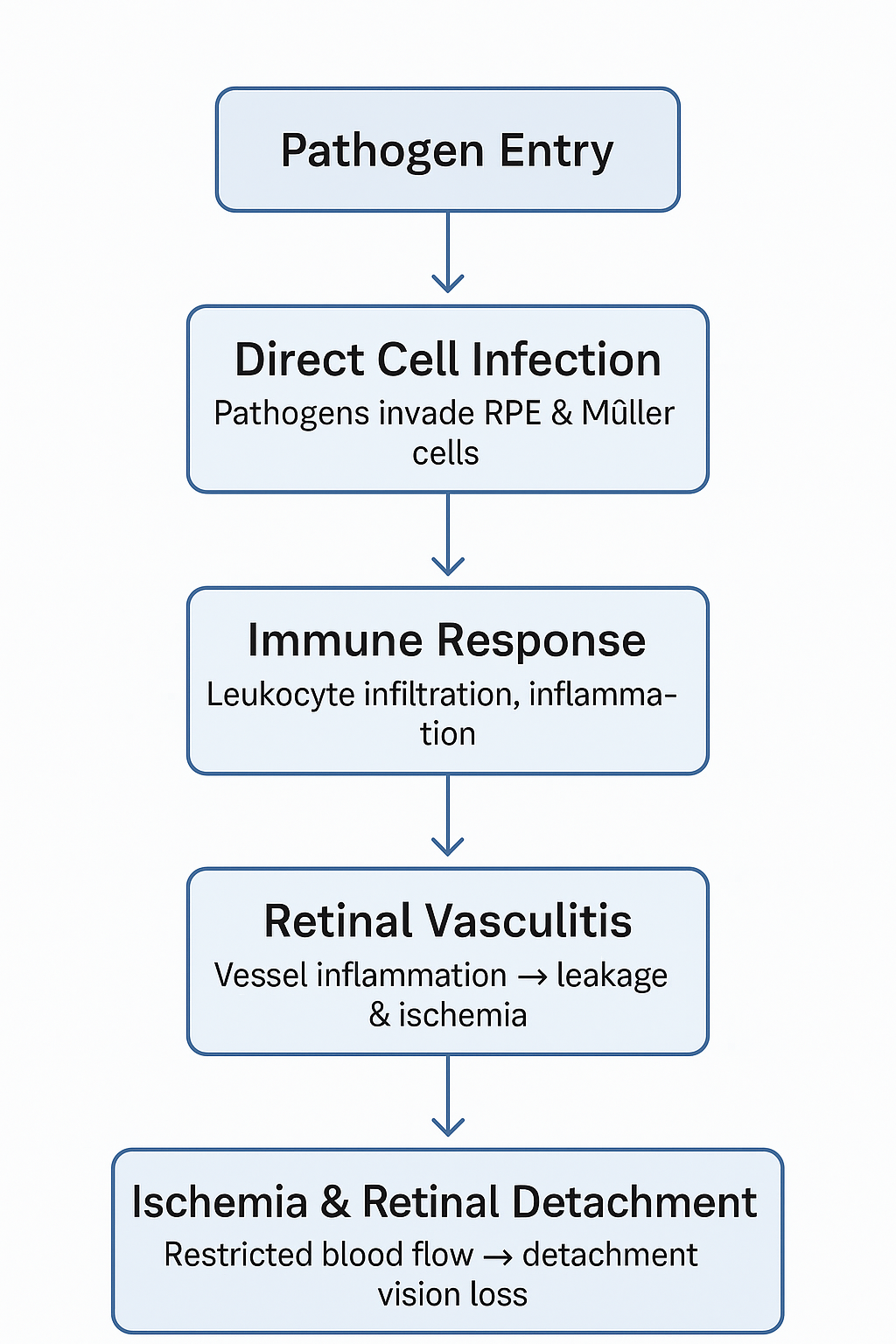
Figure 3: Flow Chart Showing the Pathophysiology of Retinitis
Metabolic and Vascular Disorders
Diabetes and hypertension commonly cause retinal microvascular changes. Diabetic retinopathy and hypertensive retinopathy are classic examples where fundus findings guide both diagnosis and management. The degree of retinal involvement often mirrors systemic vascular injury, alerting clinicians to the risk of complications such as kidney and cardiovascular damage. (1,4)
Other Conditions
Pre-eclampsia / Eclampsia: In obstetric settings, fundus changes may assist in risk assessment and management, helping predict adverse outcomes for the mother and foetus. (5)
Neurological Disorders: Optic disc changes can indicate raised intracranial pressure or neurodegenerative processes, supporting broader neurological evaluation. (1)
Clinical Application and Broader Impact
Routine or targeted fundus examination is especially valuable in:
- Patients with systemic infectious disease screening can detect clinically significant ocular involvement, even when patients are asymptomatic. (2)
- Chronic disease management findings can support diagnosis, grading of severity, and monitoring of treatment efficacy. (3)
- Multiple settings techniques such as ophthalmoscopy, colour fundus photography, and optical coherence tomography (OCT) allow detailed visualisation and can be used in bedside care or resource-limited environments. (2)
Conclusion
Fundus examination remains a powerful yet often under-utilised tool in systemic disease management. By revealing early and sometimes silent signs of systemic illness, it enables timely, targeted interventions that can improve outcomes across a wide spectrum of diseases. Its non-invasive nature and diagnostic strength highlight the importance of fundus screening in both ophthalmic and general clinical practice. (1,3)
References
- Schneiderman, H. (1990). The funduscopic examination. In H. K. Walker, W. D. Hall, & J. W. Hurst (Eds.), Clinical methods: The history, physical, and laboratory examinations (3rd ed., Chap. 117). Butterworths.
- Visioli, G., Zeppieri, M., Iannucci, V., Manni, P., Albanese, G. M., Salati, C., Spadea, L., & Pirraglia, M. P. (2023). From bedside to diagnosis: The role of ocular fundus in systemic infections. Journal of Clinical Medicine, 12(23), 7216.
- Meng, L., Wang, Y., Yang, Z., Lin, S., Wang, Y., Chen, H., … & Chen, Y. (2024). Ocular fundus changes and association with systemic conditions in systemic lupus erythematosus. Frontiers in Immunology, 15, 1395609.
- Kumar, S., Kiran, N., & Mahato, R. K. (2024). Ocular Manifestations of Systemic Diseases: Implications for Comprehensive Patient Care. Journal of Pharmacy and Bioallied Sciences, 16(Suppl 3), S2854–S2856.
- Divyaa, M., Mohanapriya, P., Jeevakala, C., & Priyadharshni, S. (2024). Study of ocular fundus changes in obstetric cases with underlying systemic disease. Int J Acad Med Pharm, 6(4), 307–311.
About the Author


Recent Comments