Narmadha R, M. Optom.
Assistant Professor, Dhanalakshmi Srinivasan University, Trichy, India
A scleral lens is a large-diameter medical device that completely covers the cornea, protecting it with a fluid reservoir. This creates an ideal ocular surface environment and makes these lenses particularly useful for ocular surface disorders. The overall goal when prescribing scleral lenses for ocular surface disorders is to improve comfort while supporting the ocular surface and improving clinical signs of ocular surface disorders. (1)
Ocular Surface Disorder
Ocular Surface Disorder (OSD) is a multifactorial disorder of conjunctival epithelium, corneal epithelium, lacrimal glands, and meibomian glands that results in either deficient or inappropriate tear production and leads to decreased visual clarity and ocular discomfort through various inflammatory pathways. (2)
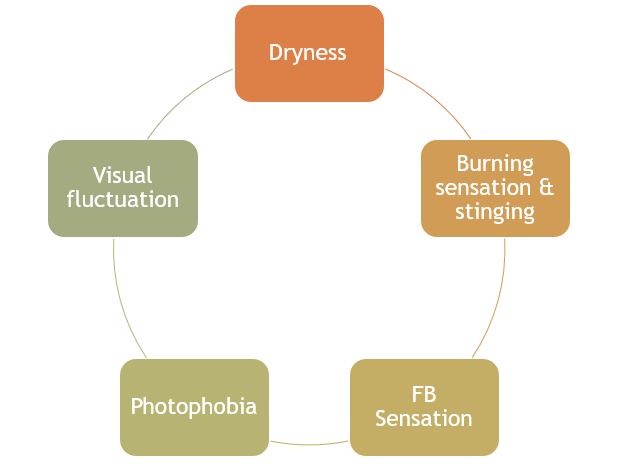
Figure 1: Symptoms of Ocular Surface Disorder (OSD)
Benefits
Scleral lenses can be a good treatment option for Ocular Surface Disorders (OSD) because they can:
- Protect the eye: Scleral lenses vault the cornea instead of sitting on it, which can help minimise irritation and damage.
- Lubricate the eye: Scleral lenses are custom fit to lubricate the surface of the eyes.
- Improve vision: Scleral lenses can provide optimal visual correction.
- Reduce discomfort: Scleral lenses can decrease pain, itchiness, eye redness, and the need to rub the eyes or apply eye drops. (1)
Efficacy of Scleral Lens in Ocular Surface Disorders
1. Dry Eye:
A recent presentation at the Global Speciality Lens Symposium compared lens comfort and Dry Eye Disease (DED) symptoms in scleral lens wearers with Hydra-PEG-treated lenses to those with untreated scleral lenses. Patients with Hydra-PEG-treated scleral lenses reported increased comfort and improved dry eye symptoms than those with untreated lenses. (1)
2. Stevens-Johnson Syndrome:
A study reported that the Prosthetic Replacement of the Ocular Surface Ecosystem (PROSE) scleral lenses would offer improvements in visual acuity and function for patients with chronic ocular manifestations of Stevens-Johnson Syndrome (SJS) who had failed conventional treatments. (3)
3. Graft vs Host Disease:
A study discovered that a scleral lens is a good option for treating ocular Graft vs Host Disease (GVHD) because the liquid reservoir beneath the lens allows for continuous hydration of the ocular surface, protecting against evaporation and aiding in the resurfacing of the damaged corneal epithelium, possibly by reducing tear film hyper-osmolarity. (1)
4. Graft vs Host Disease:
A study found that the scleral contact lens was effective in promoting the healing of persistent corneal epithelial defects in some eyes that failed to heal after other therapeutic measures. (4)
5. Exposure keratopathy:
A study reported that restoration of corneal integrity and clarity was achieved with the aid of therapeutic scleral lenses, and they were found to be a highly effective treatment modality for patients. (5)
Conclusion
Scleral lenses represent a significant advancement in the treatment of ocular surface disorders, addressing both therapeutic and visual rehabilitation needs. Their unique design creates a protective and hydrating environment, making them invaluable for managing severe dry eye, irregular corneas, and post-surgical recovery. Scleral lenses have transformed the quality of life for patients with complex ocular conditions.
References
- Harthan, J. S., & Shorter, E. (2018). Therapeutic uses of scleral contact lenses for ocular surface disease: patient selection and special considerations. Clinical optometry, 10, 65–74. https://doi.org/10.2147/OPTO.S144357.
- Zhang, X., Vadoothker, S., Munir, W. M., & Saeedi, O. (2019). Ocular Surface Disease and Glaucoma Medications: A Clinical Approach. Eye & contact lens, 45(1), 11–18. https://doi.org/10.1097/ICL.0000000000000544.
- Heur, M., Bach, D., Theophanous, C., & Chiu, G. B. (2014). Prosthetic replacement of the ocular surface ecosystem scleral lens therapy for patients with ocular symptoms of chronic Stevens-Johnson syndrome. American journal of ophthalmology, 158(1), 49–54. https://doi.org/10.1016/j.ajo.2014.03.012
- Rosenthal, P., Cotter, J. M., & Baum, J. (2000). Treatment of persistent corneal epithelial defect with extended wear of a fluid-ventilated gas-permeable scleral contact lens. American journal of ophthalmology, 130(1), 33–41. https://doi.org/10.1016/s0002-9394(00)00379-2
- Grey, F., Carley, F., Biswas, S., & Tromans, C. (2012). Scleral contact lens management of bilateral exposure and neurotrophic keratopathy. Contact lens & anterior eye : the journal of the British Contact Lens Association, 35(6), 288–291. https://doi.org/10.1016/j.clae.2012.07.009
- Schornack, M. M., Pyle, J., & Patel, S. V. (2014). Scleral lenses in the management of ocular surface disease. Ophthalmology, 121(7), 1398–1405. https://doi.org/10.1016/j.ophtha.2014.01.028

Recent Comments