Anshi Jha, B. Optom
Student, Uttar Pradesh University of Medical Sciences, Saifai, India
When two patients are prescribed identical refractive corrections, their visual outcomes may still differ due to individual variations in ocular anatomy, neural adaptation, and visual processing. Clinically, one patient may achieve 6/6, while another may only reach 6/9 or 6/12 even with identical lens power. This variation can be explained by a key optical concept: the Circle of Blur. (1)
Concept of Circle of Blur
The Circle of Blur (also known as the Circle of Confusion) forms when light rays fail to focus precisely on the retina. Instead of forming a sharp point, they create a small circular disc of light.
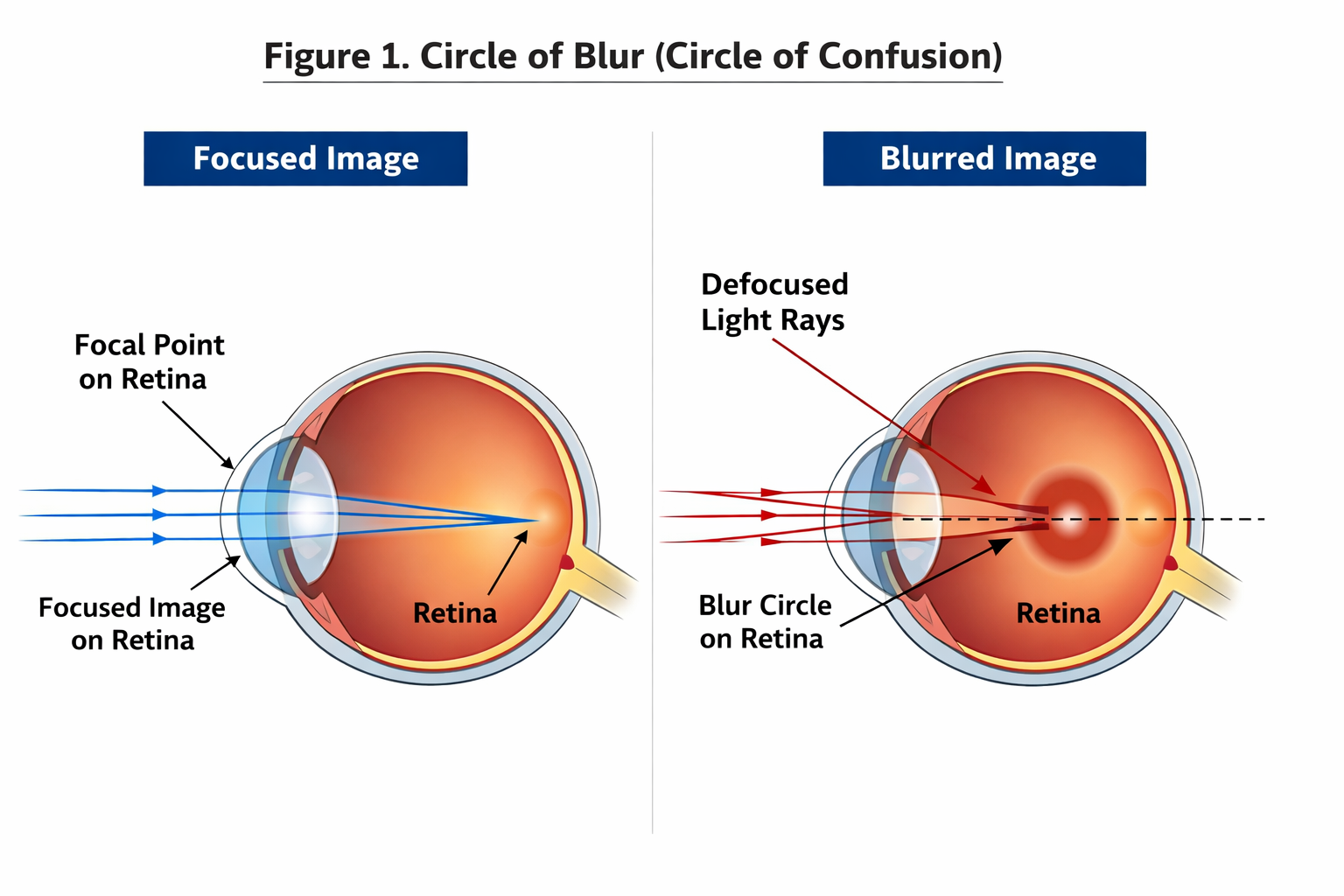
Figure 1: Pathophysiology of OSA
The larger this blur circle, the poorer the visual acuity. A larger blur circle indicates a greater degree of retinal defocus, which degrades image sharpness and reduces the eye’s ability to resolve fine details, ultimately resulting in poorer visual acuity. (2) Even a minor increase in blur circle diameter can significantly influence clarity.
Why Do Two Patients With the Same Power See Differently?
Pupil Size Differences
A larger pupil allows more peripheral and defocused rays to enter the eye, increasing the blur circle diameter and reducing acuity. (1) This explains why night vision often becomes poorer when pupils dilate.
Higher-Order Aberrations (HOAs)
Higher-order aberrations (HOAs) are optical imperfections such as spherical aberration and coma that cannot be corrected with standard spectacles. Increased HOAs enlarge the retinal blur circle by dispersing light irregularly on the retina, leading to reduced contrast sensitivity and degraded visual quality, especially under low-light conditions and with larger pupil sizes. These aberrations scatter incoming rays differently and modify the blur circle, leading to different visual outcomes despite the same lens power. (3)
Retinal and Neural Processing Variability
Two individuals may have differences in photoreceptor health, contrast sensitivity, and neural processing speed. This leads to different interpretations of the same retinal blur image, resulting in different acuity even with the same prescription. (2)
Accommodation Lag or Lead
In young or highly accommodative patients, a lag of accommodation results in Hyperopic defocus because the accommodative response is insufficient for the visual demand, causing the image to focus behind the retina, whereas a lead of accommodation produces Myopic defocus due to excessive accommodation that shifts the focal point in front of the retina. Both conditions change the blur circle size and therefore the subjective visual acuity. (1)
Tear Film Quality
A stable tear film is essential for a sharp optical interface. Dry eye or an unstable tear film causes micro-distortions on the cornea, altering the blur circle moment-to-moment and reducing visual consistency. (2)
| Factor | Effect on Blur Circle | Clinical Observation |
|---|---|---|
| Pupil size | Larger pupil increases blur diameter | Reduced night vision |
| Higher-order aberrations | Irregular light distribution | Reduced contrast sensitivity |
| Accommodation error | Focus shifts from retina | Variable clarity |
| Tear film instability | Optical surface distortion | Fluctuating vision |
| Neural processing | Altered perception of blur | Different acuity outcomes |
Table 1: Factors Influencing the Size of the Blur Circle
Clinical Relevance
Understanding the Circle of Blur helps optometrists to:
- Identify why the same refractive power does not always yield the same vision. (3)
- Fine-tune refraction endpoints through subtle adjustments to achieve maximal visual clarity and patient comfort.
- Counsel patients with ocular pathology, higher-order aberrations, or dry eye.
- Recognise that even ±0.25 D residual blur can significantly affect acuity. (3)
When a patient asks, “Why can’t I see 6/6 even with this number?” the answer often lies in the physiology of the blur circle.
Conclusion
The Circle of Blur shows that vision is the combined result of optical focus, aberrations, accommodation, tear stability, pupil size, and neural processing. This is why two patients with the same refractive correction may have different visual acuity outcomes. It reinforces the importance of tailoring refraction to each patient while considering higher-order aberrations, accommodative behaviour, and binocular interactions to ensure the clearest and most comfortable vision.
References
- Atchison, D. A., & Smith, G. (2000). Optics of the human eye. Butterworth-Heinemann.
- Rabbetts, R. B. (2007). Bennett & Rabbetts’ clinical visual optics (4th ed.). Elsevier.
- Thibos, L. N., & Hong, X. (1999). Clinical applications of the Shack–Hartmann aberrometer. Optometry and Vision Science, 76(12).
- Artal, P. (2014). Understanding aberrations by example. Journal of Optometry, 7(1).
About the Author



Recent Comments