Sheenam Wakeel, B. Optom, F. Optom
Oculoplasty Optometrist, Dr. Shroff’s Charity Eye Hospital, New Delhi, India
Cysticercosis is caused by the larval stage of Taenia solium (bacon tapeworm). Humans become infected by drinking contaminated water, eating undercooked pork, or consuming vegetables tainted with the worm’s eggs. In rare cases, eggs can travel backward from the intestine into the bloodstream, leading to auto-infection. In its life cycle, the tapeworm resides in the human intestine (definitive host) and lays eggs, which are passed in stool. Pigs (intermediate hosts) ingest these eggs, which release larvae that settle in their muscles. (1,2) When humans eat undercooked pork, the larvae infect the body, forming cysts in tissues such as muscles, brain, or eyes. When these cysts rupture, they release toxins that cause swelling, inflammation, and, over time, hard nodular formations. (4)
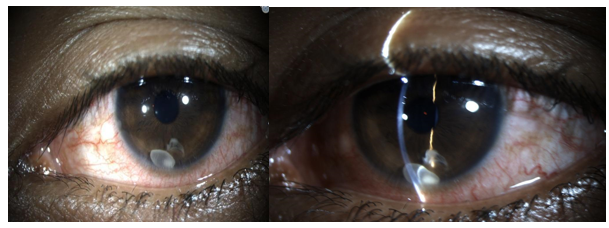
Figure 1: Cysticercosis by Slit Lamp
Anterior Segment Cysticercosis
Anterior chamber cysticercosis is a rare parasitic eye infection in which a live cyst appears in the anterior chamber, the fluid-filled space between the cornea and iris. A free-floating cyst in this area is an even rarer finding, with only a few documented cases in medical literature. (7) The exact pathway by which the cyst enters the anterior chamber remains unclear. Possible routes include migration through the pupil (especially in aphakia), via blood vessels supplying the ciliary body, or through the anterior chamber angle. (5–7)
Ocular cysticercosis primarily affects young individuals and occurs equally in both genders. (9) The cyst may attach to structures such as the iris, anterior lens capsule, or corneal endothelium through a stalk-like connection. (9) Small cysts may remain asymptomatic, whereas larger or active cysts can cause reduced vision, floaters, or leukocoria (white pupillary reflex). Pain and redness may occur due to associated iridocyclitis, inflammation of the iris and ciliary body. (9–11) Glaucoma may result either from inflammation or a pupillary block caused by the cyst. (12) Intracameral cysticercosis has also been mistaken for cataract or anterior lens dislocation. (11,12)
Diagnosis
Visual acuity, pupil examination, and Intraocular pressure assessment are important. If the cyst is in the anterior chamber, pupillary block may occur, leading to glaucoma. (9,12)
- Slit Lamp Examination: A live parasite appears as a translucent cyst measuring between 1.5 and 6 disc diameters under slit-lamp illumination. (15)
- Fundoscopic Examination: The cyst may be located within the vitreous cavity or subretinal space. It is believed to reach the vitreous via the choroidal circulation and trans-retinal migration. During retinal migration, the organism can cause exudative or rhegmatogenous retinal detachment (RRD). Although optic nerve involvement is rare, compression by the cyst may result in optic disc oedema. (16)
- Sekhar, G. C., & Lemke, B. N. (1997). Orbital cysticercosis. Ophthalmology, 104(10), 1599–1604.
- Beri, S., Vajpayee, R. B., Dhingra, N., & Ghose, S. (1994). Managing anterior chamber cysticercosis by viscoexpression: a new surgical technique. Archives of Ophthalmology, 112(10), 1279–1280.
- Aracena, T., & Roca, F. P. (1981). Macular and peripheral subretinal cysticercosis. Annals of Ophthalmology, 13(11), 1265–1267.
- Bartholowmew, R. S. (1975). Subretinal cysticercosis. American Journal of Ophthalmology, 79(4), 670–673.
- Pushker, N., Kashyap, S., Gautam, V. P., & Bajaj, M. S. (2004). Ocular cysticercosis — a profile. Tropical Doctor, 34(4), 256–256.
- DNKE-Elder, S. (1966). Diseases of uveal tract. System of Ophthalmology, 694–698.
- Mahendradas, P., Biswas, J., & Khetan, V. (2007). Fibrinous anterior uveitis due to Cysticercus cellulosae. Ocular Immunology and Inflammation, 15(6), 451–454.
- Takkar, B., Chandra, P., Kumar, K., & Vanathi, M. (2014). Toxic granulomatous anterior uveitis in live intracameral cysticercosis masquerading as leukocoria. Canadian Journal of Ophthalmology, 49(6), e140–e141.
- Chandra, A., Singh, M. K., Singh, V. P., Rai, A. K., Chakraborty, S., & Maurya, O. P. S. (2007). A live cysticercosis in anterior chamber leading to glaucoma secondary to pupillary block. Journal of Glaucoma, 16(2), 271–273.
- Kapoor, S., Sood, G. C., Aurora, A. L., & Sood, M. (1977). Ocular cysticercosis: report of a free-floating cysticercus in the anterior chamber. Acta Ophthalmologica, 55(6), 927–930.
- Goyal, J. L., Das, S., Kumar, S., Chauhan, D., Baheti, U., & Sangit, V. (2007). Retrobulbar cysticercosis masquerading as optic nerve glioma. Orbit, 26(1), 61–63.
- Dhiman, R., Devi, S., Duraipandi, K., Chandra, P., Vanathi, M., Tandon, R., & Sen, S. (2017). Cysticercosis of the eye. International Journal of Ophthalmology, 10(8), 1319.
- Proaño, J. V., Madrazo, I., Avelar, F., López-Félix, B., Díaz, G., & Grijalva, I. (2001). Medical treatment for neurocysticercosis characterized by giant subarachnoid cysts. New England Journal of Medicine, 345(12), 879–885.
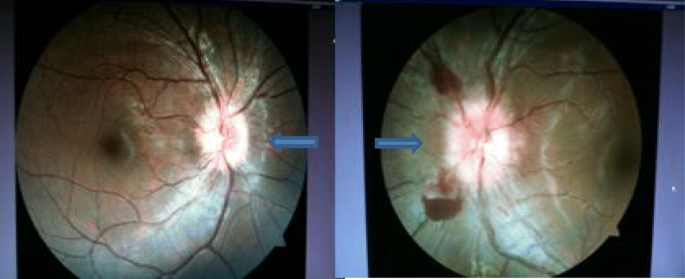
Figure 2: Fundus Photograph: Bilateral blurred, elevated disc margins and tortuous dilated vessels with parapapillary haemorrhage in the left eye (arrows).
Management
Medical Therapy: Cyst removal helps prevent complications such as vitritis, proliferative vitreoretinopathy (PVR), glaucoma, and phthisis. (17) Neurocysticercosis and orbital cysticercosis are managed with albendazole (15 mg/kg) for 4 weeks and tapered steroids (1.5 mg/kg). Steroids alone may be used when no scolex is present or when ELISA results are negative. (18–20)
Surgery: Vitrectomy is preferred over laser photocoagulation for intravitreal or subretinal cysts, as it minimizes inflammation from cyst rupture. (9)
Conclusion
Cysticercosis is a preventable disease. Avoiding undercooked or raw pork, maintaining proper hygiene, and ensuring safe food handling are key preventive measures. (21) Ocular and orbital cysticercosis can present in varied forms, but modern imaging enables accurate diagnosis even in non-endemic regions. Early detection and prompt treatment are essential for favorable visual outcomes.
References

Recent Comments