Anik Dingal, B. Optom
M. Optom Student, Vidyasagar College of Optometry and Vision Science, Kolkata, India
Several studies suggest that the gut microbiome may influence eye health, with imbalances linked to conditions such as Dry Eye, Blepharitis, allergies, and autoimmune disorders, potentially informing future treatment strategies. (1) This blog examines the relationship between the gut and the eyes, the scientific research supporting this connection, and how this insight could reshape approaches to ocular disorders in the future.
Ocular Surface Disease (OSD)
The ocular surface includes the cornea, conjunctiva, tear film, meibomian glands, and eyelids. Diseases affecting these structures are collectively known as Ocular Surface Disease (OSD). Symptoms include burning, redness, blurred vision, light sensitivity, eyelid twitching, and epiphora. (3)
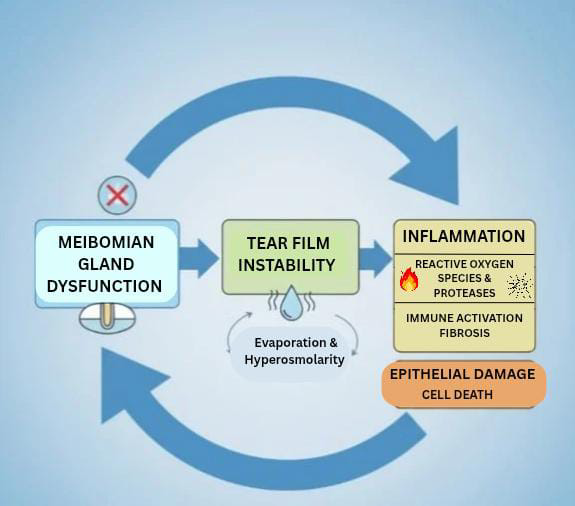
Figure 1: Pathophysiology of Ocular Surface Disease
Gut Microbiome
The gut microbiome is made up of a variety of bacteria found in the intestines that boost immunity, control inflammation, aid in the digestion of fibre, and generate vitamins B12 and K. (4) Maintaining a balanced microbiome is vital for overall health, while imbalances known as dysbiosis can lead to inflammation.(5)
| Ocular Condition | Gut-Related Findings | Proposed Mechanism |
|---|---|---|
| Dry Eye Syndrome | Reduced gut bacterial diversity, particularly in autoimmune conditions like Sjögren’s syndrome | A decrease in beneficial gut bacteria disrupts the balance of anti-inflammatory and pro-inflammatory molecules. |
| Blepharitis | Association with Gastrointestinal (GI) disorders such as Rosacea and Gastroesophageal Reflux Disease (GERD) | Dysregulation in the gut–skin–eye axis alters lipid metabolism and increases local inflammation around the eyelids and meibomian glands, contributing to chronic blepharitis. |
| Allergic Conjunctivitis | Increased Firmicutes/Bacteroidetes ratio in the gut microbiome | This imbalance enhances allergic immune responses by increasing Th2-type cytokine activity, making the ocular surface more prone to allergic inflammation. |
Table 1: Gut Microbiome and Ocular Surface Disease Association
(2)
Scientific Evidence
| No. | Author(s) & Source | Year | Topic / Focus | Key Findings | Mechanistic Insight / Conclusion |
|---|---|---|---|---|---|
| 1 | Campagnoli, L. I. M., et al. International Journal of Molecular Sciences |
2023 | Gut–eye axis strategies | Describes therapeutic potential of targeting gut microbiome for ocular diseases | Modulating gut microbiota can influence ocular inflammation |
| 2 | Tîrziu, A. T., et al. Journal of Clinical Medicine |
2024 | Microbiome imbalance and ocular diseases | Links gut dysbiosis to various ocular pathologies | Dysbiosis triggers inflammatory and immune-mediated pathways |
| 3 | Watane, A., et al. BMJ Open Ophthalmology |
2022 | Microbiome and immune-mediated dry eye | Reviews role of microbiome in immune dysregulation in dry eye | Dysbiosis → immune activation → ocular surface damage |
| 4 | Chiang, M. C., & Chern, E., et al. Frontiers in Microbiology |
2022 | Ocular surface microbiota and probiotics | Explores potential of probiotics in ocular infectious diseases | Probiotics may help restore microbiota balance and reduce pathogen load |
| 5 | Thakur, S., & Sheppard, J. D., et al. Eye & Contact Lens |
2022 | Gut microbiome and ocular surface diseases | Summarises gut–eye connection in ocular surface disorders | Altered microbiota may influence tear film and ocular surface immunity |
Table 2: Summary of Key Literature on the Gut–Eye Axis
The Gut–Eye Axis: Bridging Two Distant Organs
The gut and the eye may communicate through immune signalling pathways, microbial metabolites, and systemic inflammatory mechanisms. Key proposed links include:
Immune Regulation: Gut microbiota influence immune responses via Gut-associated Lymphoid Tissue (GALT). Immune cells activated in the gut can circulate systemically, including to ocular tissues. (11)
Systemic Inflammatory Response: Dysbiosis may promote a pro-inflammatory state that affects the ocular surface. It can also contribute to translocation of endotoxins such as lipopolysaccharides (LPS) into the bloodstream, leading to endotoxemia. (12)
Metabolites and Barrier Function: Gut bacteria produce Short-chain Fatty Acids (SCFAs) such as butyrate and acetate, which may influence inflammation and epithelial barrier integrity, potentially affecting ocular surface health. (13)
Therapeutic Considerations
1. Probiotics and Prebiotics: Oral probiotics may help restore microbial balance and reduce inflammatory signalling. Prebiotics (e.g., oligosaccharides) serve as substrates that nourish beneficial gut bacteria. (14)
2. Faecal Microbiota Transplantation (FMT): FMT is being evaluated for potential use in autoimmune and inflammatory diseases, with emerging interest in its possible role across ocular inflammatory conditions. (15)
3. Drug Adjustment: Metformin has been reported to influence gut microbial composition by promoting beneficial bacteria such as Akkermansia muciniphila and SCFA-producing species, while reducing certain pro-inflammatory taxa. It may improve glycaemic control via microbiome-mediated pathways, including enhanced insulin sensitivity and increased GLP-1 secretion, while also supporting intestinal barrier function and reducing systemic inflammation. (16)
Conclusion
In summary, the gut microbiome controls immunity, metabolism, and epithelial barrier function, all of which are critical for the health of the ocular surface. In addition to raising the risk of ocular surface problems, gut dysbiosis can encourage systemic inflammation. A viable therapeutic strategy is to restore microbial equilibrium with probiotics, prebiotics, and nutritional treatments, emphasising the gut–eye axis as a crucial area for future study and clinical treatment.
References
- Shibata, S., & Yamada, K. (2021). Gut microbiota on eye diseases: An overview. Annals of Medicine, 53(1), 750–761.
- Petrillo, F., et al. (2020). Current evidence on the ocular surface microbiota and related diseases. Microorganisms, 8(7), 1033.
- Golden, M. I., Meyer, J. J., Zeppieri, M., et al. (2025). Dry eye syndrome. In StatPearls.
- Conlon, M. A., & Bird, A. R. (2014). Diet and lifestyle impact on gut microbiota and human health. Nutrients, 7(1), 17–44.
- Zhao, M., et al. (2023). Immunological mechanisms of inflammatory diseases caused by gut microbiota dysbiosis. Biomedicine & Pharmacotherapy, 164, 114985.
- Campagnoli, L. I. M., et al. (2023). Targeting the gut–eye axis. International Journal of Molecular Sciences, 24(17), 13338.
- Tîrziu, A. T., et al. (2024). From gut to eye: Role of microbiome imbalance. Journal of Clinical Medicine, 13(18), 5611.
- Watane, A., et al. (2022). Microbiome and immune-mediated dry eye. BMJ Open Ophthalmology, 7(1), e000956.
- Chiang, M. C., & Chern, E. (2022). Ocular surface microbiota and probiotics. Frontiers in Microbiology, 13, 952473.
- Thakur, S., & Sheppard, J. D. (2022). Gut microbiome influence on ocular surface diseases. Eye & Contact Lens, 48(7), 278–282.
- Lin, P. (2019). Intestinal microbiota in ocular inflammatory diseases. Clinical & Experimental Ophthalmology, 47(4), 418–422.
- Bu, Y., et al. (2021). Gut microbiome alterations in ocular immunopathogenesis. Journal of Clinical Medicine, 10(20), 4694.
- Gupta, P. K., et al. (2021). Meibomian gland dysfunction perspective. Clinical Ophthalmology, 15, 4399–4404.
- Hemarajata, P., & Versalovic, J. (2013). Effects of probiotics on gut microbiota. Therapeutic Advances in Gastroenterology, 6(1), 39–51.
- Ebrahimi, R., et al. (2024). FMT for glaucoma: A potential strategy. Current Research in Microbial Sciences, 7, 100314.
- Yu, D., et al. (2021). Implications of gut microbiota in complex diseases. International Journal of Molecular Sciences, 22(23), 12661.
About the Author


Recent Comments